A fracture exposes cracks in Switzerland’s hospital system

A Swiss senior shares how she was bounced from hospital to hospital for a straightforward problem, experiencing issues plaguing the country’s healthcare system along the way.
With a slow but even gait, she makes her way up the gentle incline of a country lane. Her classy silk scarf and elegant loafers are a contrast to the faint smell of manure.
“I love this view,” she says, pointing out the snowy Alps in one direction, and the smoky Jura mountains in the other. It’s likely thanks to her longtime habit of walking that Margrit Suter* has recovered so well from the fracture she suffered last summer.
But before she could start to recover properly, she spent 12 nights in three different Bern area hospitals. The mismanagement of her case reflects some of the issues facing the Swiss hospital system, such as chronic understaffing and pressure to reduce costs.

More
Health and emergencies
‘Not much time to listen’
Suter had fallen and sustained a femoral neck break, requiring surgery on her upper thigh at Lindenhof HospitalExternal link in Bern the next day. Though weary and in pain, she quickly noticed that the nurses were stressed. Someone told her that the workload was 16 patients per nurse – a claim that the hospital would neither confirm nor deny, saying it was unable to comment on Suter’s stay.
Understaffing is a chronic problem in Swiss hospitals and care homes; in late 2018, Swiss public television, SRFExternal link, reported that there were 11,000 vacant nursing jobs in Switzerland. By 2030, the Swiss Association of NursesExternal link expects that figure to rise to 65,000. International studiesExternal link comparing Swiss care with that abroad have cited the “dependence of the [Swiss] system on medical staff trained abroad” as problematic.
“They didn’t have much time to listen,” says Suter, who also has a heart condition requiring several medications per day. “I nearly fainted with pain when they had me sit on the edge of the bed – but the therapist just acted like I wasn’t making enough of an effort,” she recalls.
What’s more, Suter says she was “barely off the operating table” when her case manager “barged in” to announce that she’d be moved to SiloahExternal link – a suburban hospital with a geriatric clinic – in three days. In 2017, the Lindenhof Group and SiloahExternal link announced that they had formed a “strategic cooperation” and that Siloah was “further expanding its position in geriatric medicine”.
‘Parked in the hallway’
But at Siloah, they weren’t ready for Suter, who says that when she arrived by ambulance, a staff member helped her into a wheelchair and then “parked” her in a hallway. She waited there for hours – from about 11:30am until 3:30pm – because there weren’t any beds available.
“It was the first time in my life that I felt like I had nobody who would take care of me,” she says, still shaken by the experience. Once settled in her room, Suter says it was difficult to summon a staff member – say for a sleeping pill or help to use the restroom. She says she and other patients waited up to ten minutes after ringing the buzzer. She also heard of one man who couldn’t hold it any longer and ended up breaking his hip when he tried to get up on his own.
“You get the feeling nobody’s coming and have no idea who to contact. You’re totally at their mercy. It’s just dreadful – especially if you can’t move,” says Suter.
Suter insisted on leaving Siloah after just one night and was transferred by ambulance (again) to Hirslanden Klinik Beau-SiteExternal link in Bern. Her expensive heart medication never made it, despite the fact that it was labelled with her name. Siloah has not responded to SWI’s request for more information about Suter’s case.
At Beau-Site, the situation was much better, says Suter. And though she had the impression that the personnel were rather overworked – with caseloads ranging from three to ten patients per staff member – she appreciated that they always took the time to introduce themselves and explain what shift they were on.
It’s not just the number of nursing staff that’s declining in Switzerland, but also that of hospitals. In 1998, there were 378; by 2017 there were 281. The reduction represents a mixture of closures and mergers undertaken to improve cost-effectiveness.

More
Swiss spend the most on healthcare
Cutting costs
Suter says her doctor apologized for the bad experience she had, and the mishaps that occurred. He blamed it on the pressure to keep costs down.
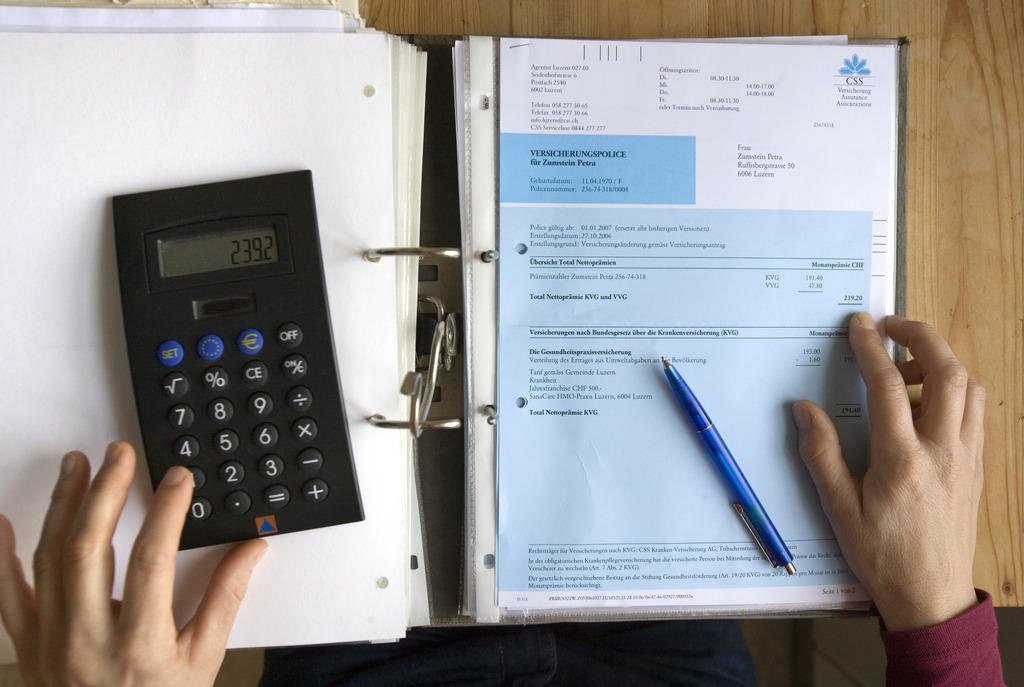
Swiss health care is among the most expensive in the world, with economists predicting that the per-person cost will be over CHF10,000 ($10,017) per year in 2018 and 2019. According to the federal cost oversight officeExternal link, about 13% of the Swiss GDP goes towards healthcare, with spending rising five times faster than salaries.
Health2020External link, a federal strategy to improve the system, states that “the services currently available could be provided around 20% less expensively with no loss of quality”. To achieve this, it suggests measures like promoting the use of generic drugs and putting more emphasis on flat-rate fees rather than item-of-service fees to discourage unnecessary services and treatments.
Suter recovered after two weeks at a rehabilitation clinic in the Bernese Oberland followed by physiotherapy within walking distance of her home. Now she stretches her legs whenever she can – just as she always did.
“It’ll never be the same, but I’m content,” she says. “Still, it makes me sick to think of the patients who can’t speak up for themselves.”
* Name changed

More
Swiss rated third in health services quality survey

In compliance with the JTI standards
More: SWI swissinfo.ch certified by the Journalism Trust Initiative




You can find an overview of ongoing debates with our journalists here. Please join us!
If you want to start a conversation about a topic raised in this article or want to report factual errors, email us at english@swissinfo.ch.